One of the most exciting developments in replacing animal testing is what we refer to as ‘cell cultures’ or ‘organs on a chip’.
These got a huge boost in the arm from the HELA cells (a fascinating story – read about it in this book, and thanks Trish for the introduction – “The Immortal Life of Henrietta Lacks” https://www.amazon.com/Immortal-Life-Henrietta-Lacks/dp/1400052181, or watch the movie at Neon).
HeLa cells (which were the very aggressive cervical cancer cells of Henrietta Lacks. taken in 1951), were the first cells to grow in a lab (in vitro), and have since provided many many trillions of cells as a base for research (it is estimated over 50 tons of cells have been cultivated). HeLa cells, like other cell lines, are termed "immortal" in that they can divide an unlimited number of times in a laboratory cell culture plate as long as fundamental cell survival conditions are met (i.e. being maintained and sustained in a suitable environment.)
The cells have been used in the following types of research, cancer, AIDs, effects of radiation and toxic substances, gene mapping and countless other scientific pursuits. Of particular note was their use in the eradication of polio, and taming various viruses.
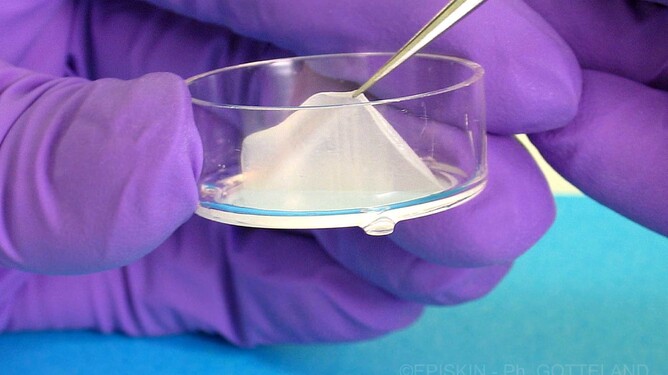
HeLa cells and other immortal cells are grown in vitro in petri dishes and used to test drugs and other treatments (eg radiation) instead of using animals as the testing environment.
Here are some of the current leading ways that cell culture is used:
Cell culture and tissue engineering (MPS – Microphysiological engineering)
1. In-vitro cell culture technique tests. The Beiersdorf 3T3-Neutral Red Uptake phototoxicity test for compatibility of new ingredients under the influence of UV light is the global standard and the first in-vitro test that was also recognised in China.
2. Organoids – 3D cell cultures grown from stem cells in a dish resembling miniature human organs: heart organoids beat like the real thing. These can be used to model disease and test new drugs.
Organoids are grown on scaffolds from three kinds of human or animal stem cells and can be grown to mimic the structure and function of different organs such as the Brain, Liver, Lung, Kidney and Intestines. Scientists developed mini-brain organoids to model how Covid-19 can affect the brain and how the Zika virus disrupts foetal brain development.
Organoids have also been used in modelling genetic diseases such as cystic fibrosis, neurodegenerative diseases like Alzheimers and Parkinsons.
3. Tumoroids (3D cell cultures derived from cells biopsied from human patients) can be used in studying the genomics and drug resistance of tumours in different organs.
Examples exist (Lift Biosciences) where the drug treatment didn’t destroy a tumour on a mouse, but obliterated it on a tumoroid. Studies have shown that tumoroids are about 80% predictive of how effective a drug will be, far surpassing the average 8% accuracy rate in animal models.
4. Bio-Chips
These 2cm wide chips can be engraved into a series of small chambers each containing a sample of tissue from a different part of the body.
A Substitute of blood flows through micro-channels and then the test drug is injected, mimicking what goes on in the body on a micro-scale. The information is then transferred to the computer for analysis.
5. Organs on a chip – these are plastic blocks lined with stem cells and a circuit that stimulates the mechanics of an organ.
The first drug has gone into clinical trials in the US for (CIDP – chronic inflammatory demyelinating polyneuropathy which causes muscle weakness that impairs walking and hand function), based on organ chip data alone (the drug restored neuronal function).
This leads to what we see as an exciting future – personalised testing: Future (Start Up) – Patient on a chip (allowing personalised testing of drugs before administering and assessing what will be the impact of this small molecule after it is metabolised in the liver and after it crosses the blood-brain barrier and gets into the brain).